We often associate pulmonary embolism with intense chest pain and sudden shortness of breath. However, real-life cases show that many patients never experience those classic symptoms. Instead, they might complain of vague discomfort in the shoulder, abdomen, or even feel faint for no clear reason. When symptoms go unnoticed or are misattributed, the condition silently progresses. In such cases, diagnosis is delayed, and complications become harder to avoid.
Dizziness and fainting could be early signs
Imagine someone collapsing during morning prayers in Istanbul’s Fatih Camii. No trauma, no known illness. Yet, he later learns he had a large pulmonary embolism. Syncope or fainting can be one of the earliest signs in non-classic PE cases. These episodes often mimic cardiac arrhythmias or neurologic issues. In emergency settings, unless PE is considered, patients might be discharged with only basic observations. That’s where clinical suspicion matters most.
PE can mimic gastrointestinal problems
A surprising number of PE cases present with upper abdominal pain or indigestion-like discomfort. These symptoms resemble gallbladder attacks or gastritis, especially when the pain is localized to the right side. In a hospital in Ankara, a woman was scheduled for appendectomy due to severe lower abdominal pain. A routine CT scan revealed emboli in her pulmonary arteries. Her “abdominal crisis” was, in fact, a lung issue.
Persistent cough and hoarseness without infection
Sometimes, patients visit a clinic complaining of a dry cough or unusual hoarseness. These signs often trigger evaluation for upper respiratory tract infections or allergies. But in certain PE cases, irritation of the pulmonary arteries can lead to a cough that has nothing to do with infection. In Turkish coastal cities like İzmir, where allergy seasons are long, such misdiagnoses are even more frequent. Physicians need to consider vascular causes, especially if symptoms persist.
Shoulder pain and muscular discomfort as the only symptom
Can shoulder pain mean anything serious? Surprisingly, yes. Some pulmonary emboli irritate pleural surfaces, causing referred pain in the neck, shoulder, or back. This often leads to orthopedic evaluations or physiotherapy prescriptions. In Bursa, a 47-year-old carpenter with chronic shoulder pain was eventually found to have segmental PE. His “muscle problem” had nothing to do with posture or lifting but with clot formation in the legs days earlier.
When seizures aren’t neurological
In rare but dramatic presentations, PE can appear as seizure-like episodes. These are not epileptic seizures but brief convulsions triggered by sudden oxygen deprivation. A teacher from Antalya collapsed in class, shaking for seconds. Neurologists found no evidence of brain disease. It took a chest CT ordered days later to confirm PE. These rare events highlight the diversity of PE symptoms and the need to look beyond textbook presentations.
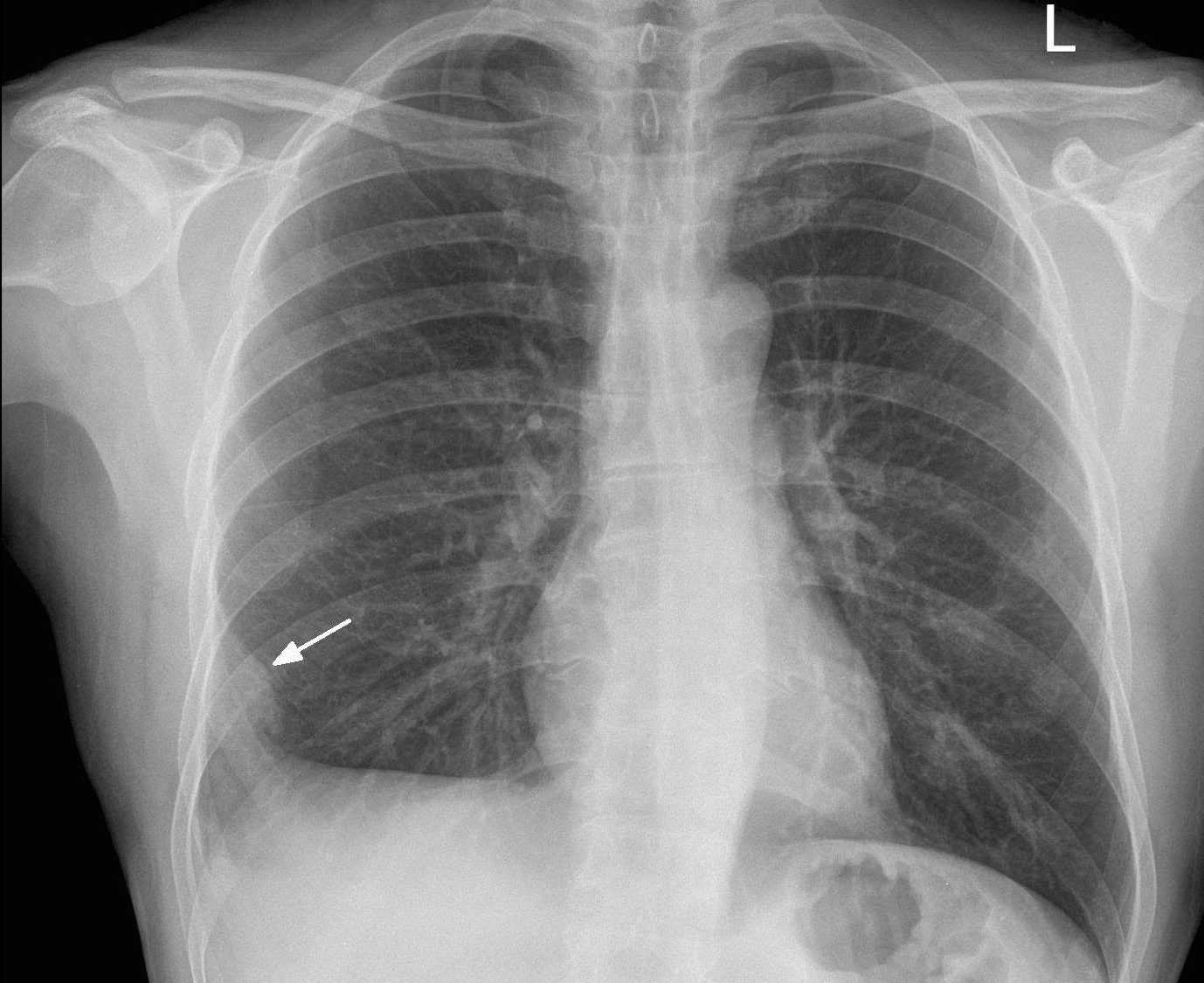
Low-grade fever can mislead diagnosis
Fever typically leads clinicians to think about infections. But pulmonary embolism can trigger an inflammatory response, causing slight fever and elevated white cell count. That misleads physicians into treating bronchitis or pneumonia, especially if the chest X-ray is clear. In Turkey’s emergency services, such overlaps often delay correct diagnosis. A febrile patient with unexplained symptoms should raise PE suspicion, not just infection alarm.
Shortness of breath may develop very late
Not all PE cases begin with breathing difficulties. In fact, shortness of breath might appear days later, when lung perfusion worsens. A middle-aged man from Gaziantep reported fatigue while climbing stairs, which he blamed on weight gain. Only after collapsing during prayer did he seek help. A CT scan revealed massive bilateral embolism. If earlier symptoms had been recognized, his outcome might have been different.
Risk factors aren’t always obvious
A major barrier to early PE diagnosis is the absence of recognized risk factors. Many patients are not post-surgery, are not on long flights, and have no known clotting issues. In a private clinic in Istanbul, a 35-year-old yoga instructor with no medical history was found to have PE. Her risk factor? A long drive to Cappadocia with minimal movement. Extended immobility, even in daily life, can quietly trigger thromboembolic events.
Vigilance saves lives—especially in silent cases
We must accept that pulmonary embolism wears many disguises. Clinicians, especially in emergency departments, must widen their differential diagnoses. Symptoms like dizziness, unexplained fever, and vague pain deserve a deeper look when initial treatments fail. In Turkish hospitals, including university centers like Hacettepe or Ege University, protocols now encourage earlier imaging when red flags appear. Every minute saved in diagnosis improves survival and reduces long-term complications.

 then "Add to Home Screen"
then "Add to Home Screen"